Mother Load: What Is Post-Natal Depletion?
‘Matrescence’, the radical transformation that occurs when a woman becomes a mother, is the biggest hormonal upheaval she can go through after adolescence. If that’s news to you, you wouldn’t be alone. So why aren’t we talking about it, frankly, all the time? And why is postpartum health generally so widely under-discussed? Here, we explore the surprising changes that accompany this transition and how to shift from surviving to thriving as a new mum.
A growing body of research suggests that pregnancy, birth and breastfeeding can profoundly – and yes, even permanently – alter a mother’s health. From shrinking the brain (turns out, baby brain isn’t just a myth) to causing a slew of nutritional deficiencies, becoming a mother can produce effects that last well past the fabled fourth trimester.
Dr Oscar Serrallach, a Byron Bay-based general practitioner and author of The Postnatal Depletion Cure, became concerned about maternal health off the back of his personal experience. “Through my own journey of having kids, I noticed a pattern of struggle with not only my partner, but a lot of my clients and friends.” Dr Serrallach explains that a mother is very different to a woman who hasn’t had children, due to the physical, emotional and social changes that occur during pregnancy and postpartum. “All her systems – nervous, hormonal, metabolic, immune – are modified; it’s a totally different landscape,” he says.
In the 1970s, anthropologist Dana Raphael created the term ‘matrescence’, a concept that’s more recently been championed by clinical psychologist Dr Aurélie Athan. Akin to adolescence, it describes the panoply of changes a woman experiences in every aspect of her life when she embarks upon motherhood.
As a society, we don’t exactly make it easy for women to thrive during matrescence. Dr Serrallach highlights the “masculinisation around motherhood” (i.e. telling mothers to “just soldier on”) as particularly harmful. “I don’t see bad mothers – I see undersupported ones,” he says. During pregnancy, mothers enjoy an abundance of attention – the seemingly endless string of medical appointments being just one example. Yet post-birth, the attention transfers almost entirely to the (admittedly adorable) baby. Add to that the myriad obligations of daily life, from careers to the hefty mental load that so often falls to women, and many women are left floundering once the congratulation cards and ‘just checking in!’ texts have dried up.
The Black Dog Institute puts the rates of perinatal depression and anxiety in Australia at around 15-20%. So Dr Serrallach coined the term ‘postnatal depletion’ to describe mothers who don’t tick the boxes for more serious conditions, but who were still on the ‘neuroinflammatory spectrum’. And just because it’s common to struggle postpartum doesn’t make it normal. “People think, “You’re a mum, you’re meant to be tired.” They don’t take it seriously,” he says.
Postnatal depletion is partly due to hormonal changes which, according to Dr Serrallach, are more significant during matrescence than during adolescence. “Researchers call it an endocrine tsunami,” he explains. And the physiological effects of becoming a mother are long-term, lasting at least seven years after the birth of a baby. High levels of inflammation during pregnancy, which can occur with gestational diabetes or hypertension, can, per Dr Serrallach, “alter a woman’s health trajectory for a very long time.” But it’s not all bad news. While it’s scary to learn that the brain shrinks during pregnancy and postpartum, as Dr Serrallach says: “The shrinkage is an upgrading: it’s cutting off dead wood. Your EQ goes up, your facial recognition and social reasoning are improved. These changes aren’t random: they’re preparing you for motherhood.”
Mothers enter a more neuroplastic state during pregnancy and the first year postpartum, which means they can learn new skills more quickly – a plus when navigating the unfamiliar territory of motherhood. But there’s a downside: “Stress is more impactful when you’re in a neuroplastic state. A sleepless night, an argument, an infection – all those kinds of things get amplified,” says Dr Serrallach.
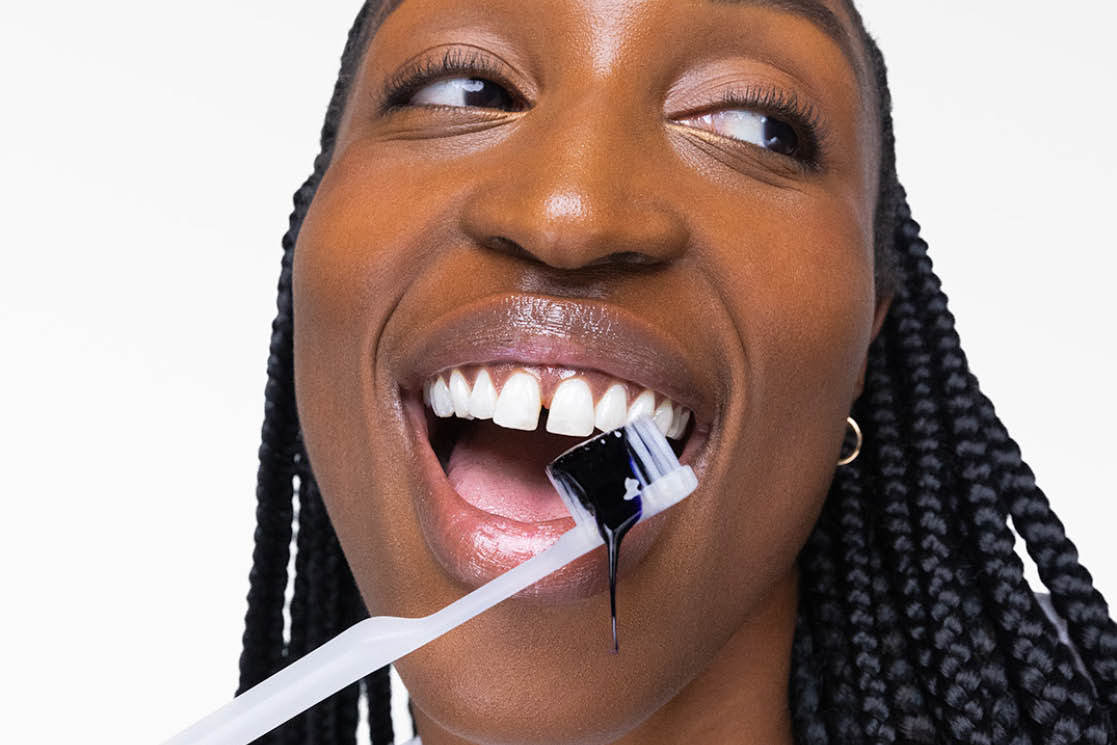
Breastfeeding impacts a woman’s health too, both positively and negatively. It has been shown to reduce a mother’s risk of developing a variety of conditions, like breast and ovarian cancer and heart disease, while other studies indicate a reduction – albeit temporary – in a lactating mother’s bone density. Postpartum health is, in Dr Serrallach’s words, “a fascinating mixed bag of plusses and minuses.”
So, How Can I Optimise My Health Postpartum?
Pregnancy can often leave women lacking in key nutrients like iron, zinc and omega-3 fats. Add in breastfeeding and barely any time or energy to prepare nutrient-dense food and you’ve got yourself a perfect storm for deficiencies. Be sure to prioritise eating well and focus on micronutrients.
A mother’s neurobiology can naturally make her feel hyper-aware 24/7, so Dr Serrallach proposes a three-tiered system to build nervous system resilience. Add in a 20-minute relaxing practice daily: think a micronap or yoga nidra. Then many 20-second moments scattered throughout the day: some deep breathing or a simple mantra like “I’m present and I’m safe.” Thirdly, one big thing once a week, such as a restorative wellness or beauty treatment – whatever is guaranteed to shift you into a relaxed state.
Prioritise your postpartum care – don’t think you can just wing it. “We have this saying: everyone prepares for the birth, but no one prepares for the postpartum,” says Dr Serrallach. “And the postpartum is so critical.” In his clinic, the gold standard for postpartum planning is deep rest for one month, deep support for 100 days and a priority on sleep for one year. An ounce of prevention is worth a pound of cure in avoiding developing more serious postnatal conditions.
Be selective about who you listen to. While advice often stems from good intentions, it doesn’t make that backhanded compliment any less hurtful. Dr Serrallach classes judgment as a ‘toxin’, so try your best to tune it out (although this is obviously easier said than done).
And finally: cut yourself some slack. “If I could kill the supermum myth – because that’s what it is, a myth – I’d be so happy,” says Dr Serrallach.
Mother Load: What Is Post-Natal Depletion?
‘Matrescence’, the radical transformation that occurs when a woman becomes a mother, is the biggest hormonal upheaval she can go through after adolescence. If that’s news to you, you wouldn’t be alone. So why aren’t we talking about it, frankly, all the time? And why is postpartum health generally so widely under-discussed? Here, we explore the surprising changes that accompany this transition and how to shift from surviving to thriving as a new mum.
A growing body of research suggests that pregnancy, birth and breastfeeding can profoundly – and yes, even permanently – alter a mother’s health. From shrinking the brain (turns out, baby brain isn’t just a myth) to causing a slew of nutritional deficiencies, becoming a mother can produce effects that last well past the fabled fourth trimester.
Dr Oscar Serrallach, a Byron Bay-based general practitioner and author of The Postnatal Depletion Cure, became concerned about maternal health off the back of his personal experience. “Through my own journey of having kids, I noticed a pattern of struggle with not only my partner, but a lot of my clients and friends.” Dr Serrallach explains that a mother is very different to a woman who hasn’t had children, due to the physical, emotional and social changes that occur during pregnancy and postpartum. “All her systems – nervous, hormonal, metabolic, immune – are modified; it’s a totally different landscape,” he says.
In the 1970s, anthropologist Dana Raphael created the term ‘matrescence’, a concept that’s more recently been championed by clinical psychologist Dr Aurélie Athan. Akin to adolescence, it describes the panoply of changes a woman experiences in every aspect of her life when she embarks upon motherhood.
As a society, we don’t exactly make it easy for women to thrive during matrescence. Dr Serrallach highlights the “masculinisation around motherhood” (i.e. telling mothers to “just soldier on”) as particularly harmful. “I don’t see bad mothers – I see undersupported ones,” he says. During pregnancy, mothers enjoy an abundance of attention – the seemingly endless string of medical appointments being just one example. Yet post-birth, the attention transfers almost entirely to the (admittedly adorable) baby. Add to that the myriad obligations of daily life, from careers to the hefty mental load that so often falls to women, and many women are left floundering once the congratulation cards and ‘just checking in!’ texts have dried up.
The Black Dog Institute puts the rates of perinatal depression and anxiety in Australia at around 15-20%. So Dr Serrallach coined the term ‘postnatal depletion’ to describe mothers who don’t tick the boxes for more serious conditions, but who were still on the ‘neuroinflammatory spectrum’. And just because it’s common to struggle postpartum doesn’t make it normal. “People think, “You’re a mum, you’re meant to be tired.” They don’t take it seriously,” he says.
Postnatal depletion is partly due to hormonal changes which, according to Dr Serrallach, are more significant during matrescence than during adolescence. “Researchers call it an endocrine tsunami,” he explains. And the physiological effects of becoming a mother are long-term, lasting at least seven years after the birth of a baby. High levels of inflammation during pregnancy, which can occur with gestational diabetes or hypertension, can, per Dr Serrallach, “alter a woman’s health trajectory for a very long time.” But it’s not all bad news. While it’s scary to learn that the brain shrinks during pregnancy and postpartum, as Dr Serrallach says: “The shrinkage is an upgrading: it’s cutting off dead wood. Your EQ goes up, your facial recognition and social reasoning are improved. These changes aren’t random: they’re preparing you for motherhood.”
Mothers enter a more neuroplastic state during pregnancy and the first year postpartum, which means they can learn new skills more quickly – a plus when navigating the unfamiliar territory of motherhood. But there’s a downside: “Stress is more impactful when you’re in a neuroplastic state. A sleepless night, an argument, an infection – all those kinds of things get amplified,” says Dr Serrallach.
Breastfeeding impacts a woman’s health too, both positively and negatively. It has been shown to reduce a mother’s risk of developing a variety of conditions, like breast and ovarian cancer and heart disease, while other studies indicate a reduction – albeit temporary – in a lactating mother’s bone density. Postpartum health is, in Dr Serrallach’s words, “a fascinating mixed bag of plusses and minuses.”
So, How Can I Optimise My Health Postpartum?
Pregnancy can often leave women lacking in key nutrients like iron, zinc and omega-3 fats. Add in breastfeeding and barely any time or energy to prepare nutrient-dense food and you’ve got yourself a perfect storm for deficiencies. Be sure to prioritise eating well and focus on micronutrients.
A mother’s neurobiology can naturally make her feel hyper-aware 24/7, so Dr Serrallach proposes a three-tiered system to build nervous system resilience. Add in a 20-minute relaxing practice daily: think a micronap or yoga nidra. Then many 20-second moments scattered throughout the day: some deep breathing or a simple mantra like “I’m present and I’m safe.” Thirdly, one big thing once a week, such as a restorative wellness or beauty treatment – whatever is guaranteed to shift you into a relaxed state.
Prioritise your postpartum care – don’t think you can just wing it. “We have this saying: everyone prepares for the birth, but no one prepares for the postpartum,” says Dr Serrallach. “And the postpartum is so critical.” In his clinic, the gold standard for postpartum planning is deep rest for one month, deep support for 100 days and a priority on sleep for one year. An ounce of prevention is worth a pound of cure in avoiding developing more serious postnatal conditions.
Be selective about who you listen to. While advice often stems from good intentions, it doesn’t make that backhanded compliment any less hurtful. Dr Serrallach classes judgment as a ‘toxin’, so try your best to tune it out (although this is obviously easier said than done).
And finally: cut yourself some slack. “If I could kill the supermum myth – because that’s what it is, a myth – I’d be so happy,” says Dr Serrallach.













Comments